︎ Health Connect:
Creating an Equitable Community Health Ecosystem
Our aim is to create hyper-localized disruptions within a community’s
existing social determinants of health for better health outcomes.
By Natalie DeLiso ︎, Nina Lang ︎, Nehal Jain ︎, Angana Symanoy ︎


Why
The medical community is increasingly incorporating a set of principles called the Social Determinants of Health into assessments of patient health. Health Connect seeks to address these social determinants both physically and digitally to decrease isolation and activate underutilized urban space. According to Michigan's 2020 Primary Care Needs Assessment, Michigan has no shortage of primary care providers, but these providers are distributed unequally and are not always utilized even within densely populated healthcare networks. This is not just a Michigan problem: 80% of counties across the United States lack healthcare access according to a 2021 GoodRx Study. [Insert project name here] aims to provide a widely applicable framework of digital and physical interventions to move communities from underutilized space and disconnected community health services to engaged and connected health ecosystems for equitable health access.

Social Determinants of Health Pyramid. Source: http://www.healthydouglas.org/
How
Health Connect's physical interventions are scalable based on the existing healthcare infrastructures of each community. While an urban area like Detroit might have an abundance of physical clinics, location-activated healthcare reminders could be built into naturally occurring urban waiting spaces like bus stops or laundromats. Suburban environments like Livingston County might require interventions such as deployable popups or mobile clinics. Finally, because of the sprawling nature of rural environments, communities such as Clare County would require the most physical of interventions, with semi-permanent clinic buildings located near other local infrastructures like libraries, post offices, or grocery stores to ensure the most access for the most people.
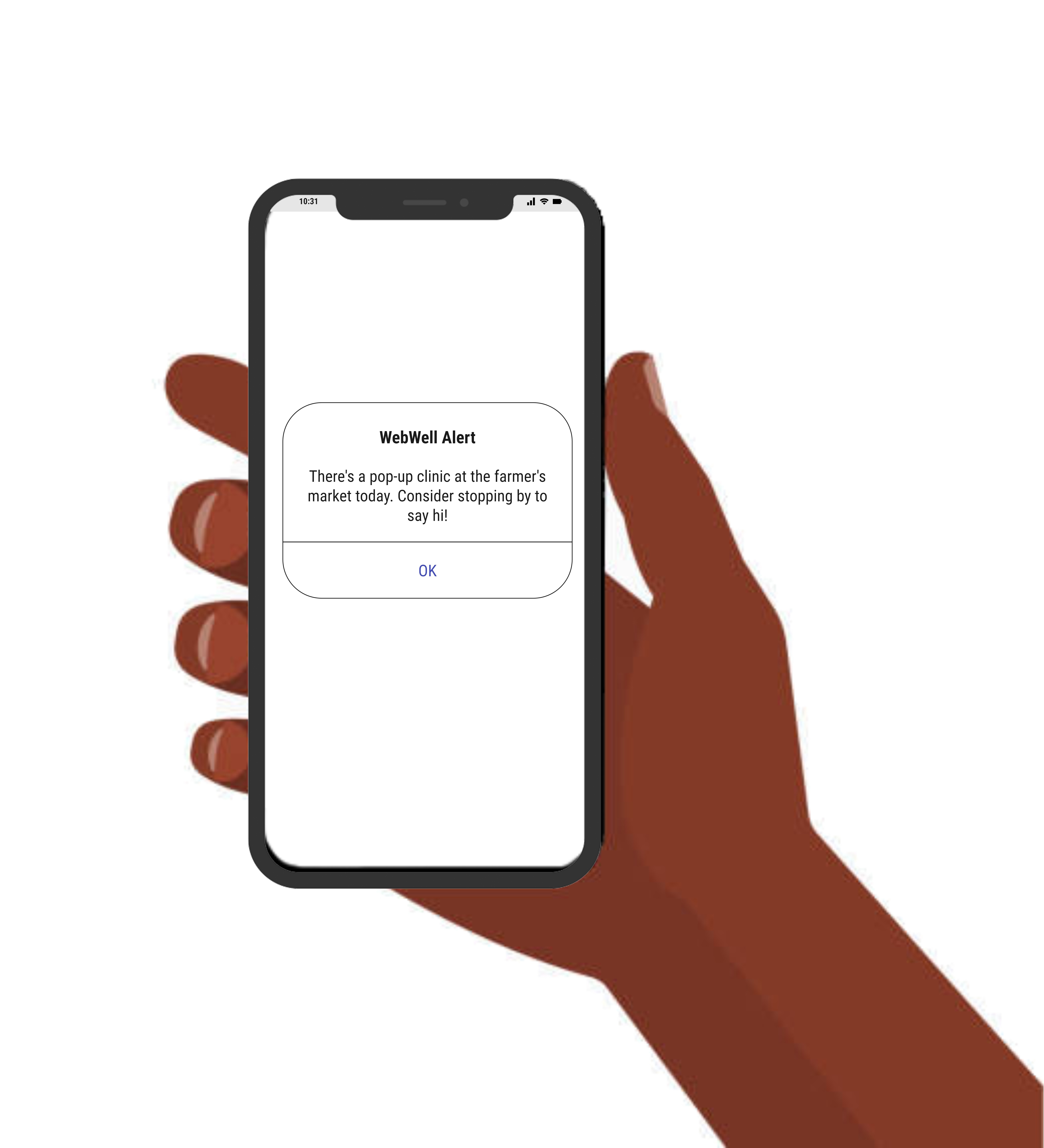
The digital interface is conceived as the secondary connection between an individual and their health community, driven by the Social Determinants of Health. A series of "check ins" is available on the app seek to address different elements of the Social Determinants: A notification nudge for a grandchild to check on their grandparent who hasn't logged their medication intake in several days would address the "Social and Community Context" Determinant, for example. These digital interventions also become physical when addressing the "Healthcare Access" and "Neighborhood and Built Environment" Determinants with invitations to local popup health screenings, EMR tech literacy classes, and insurance enrollment drives.
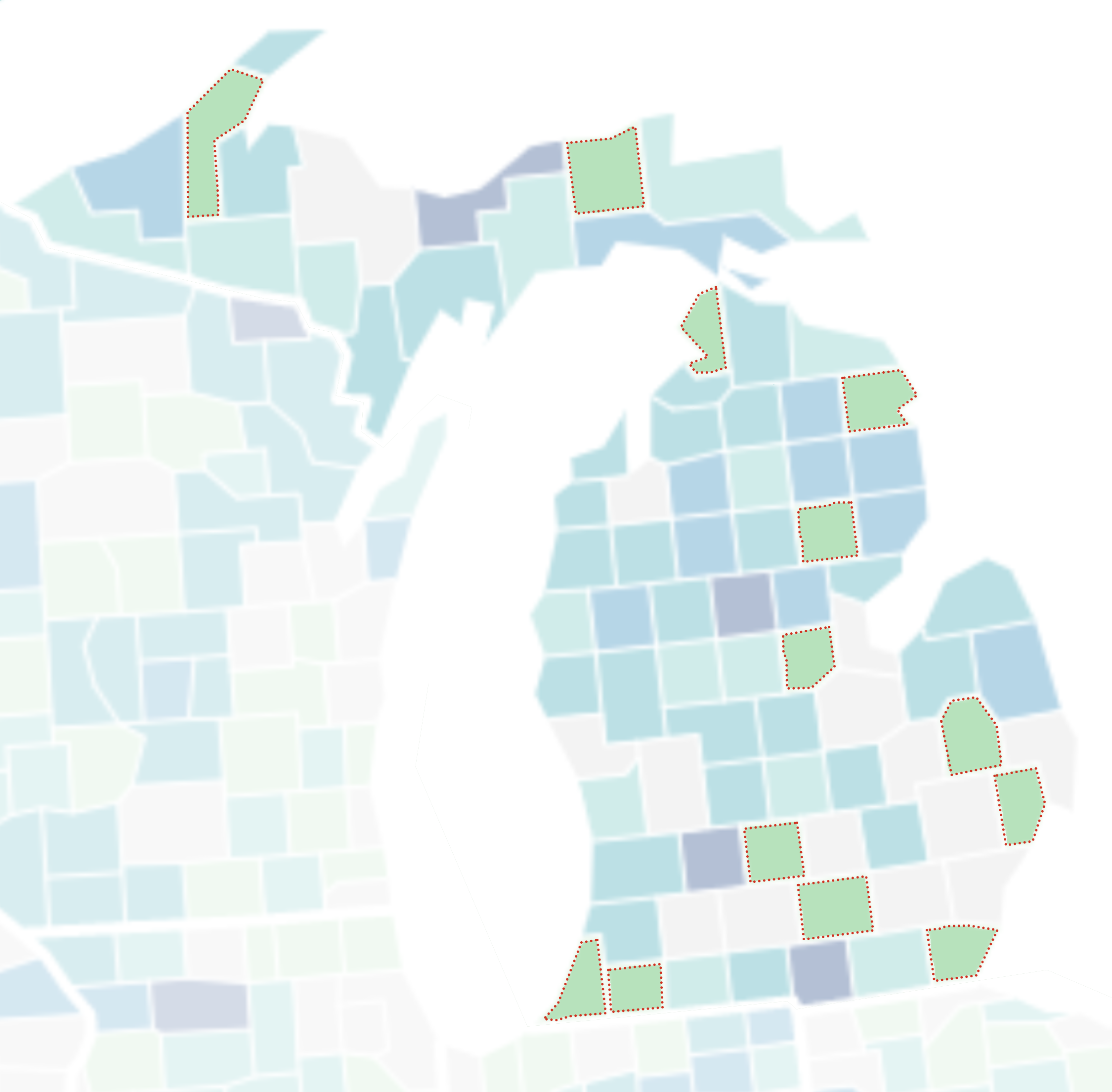
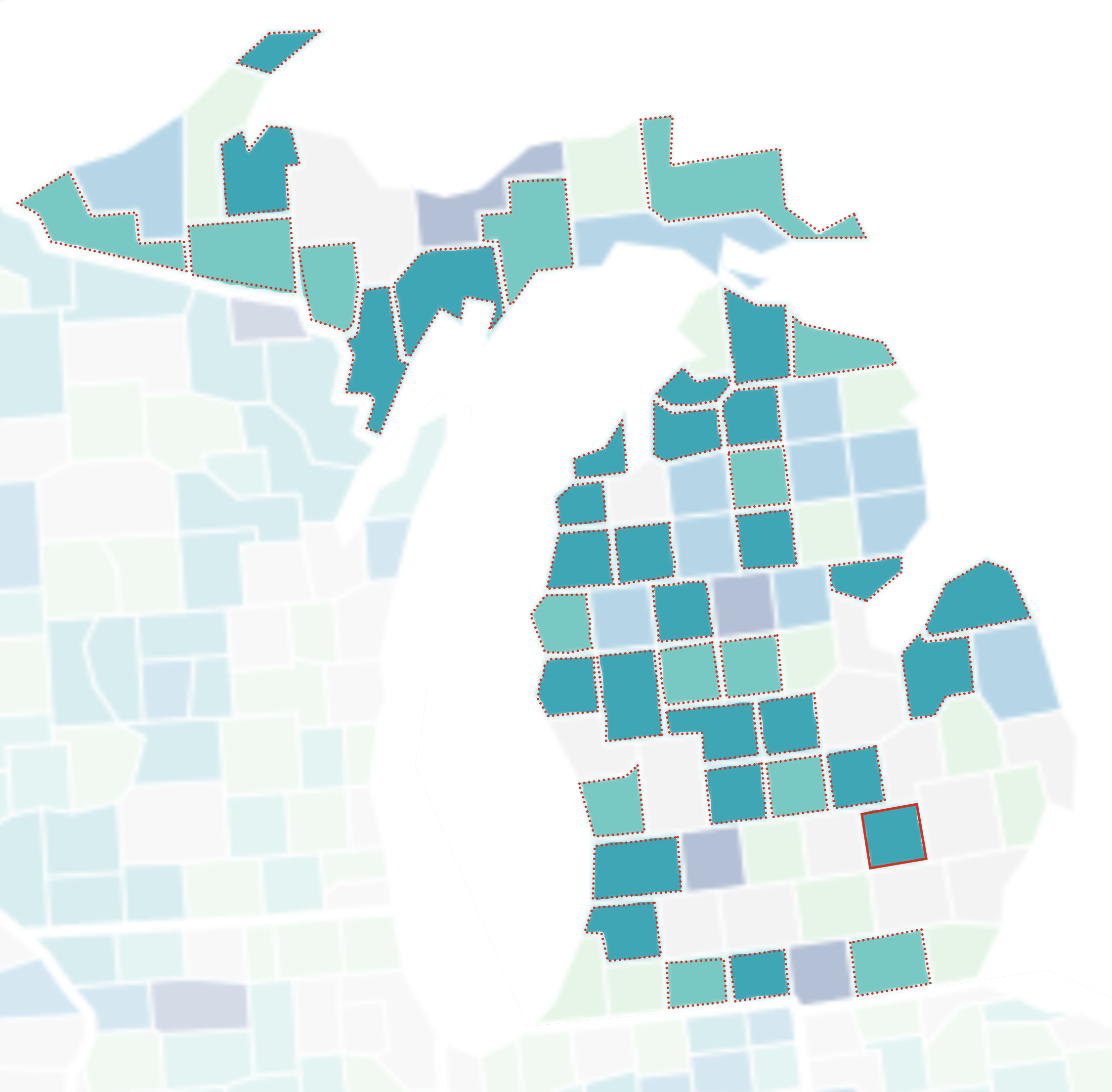
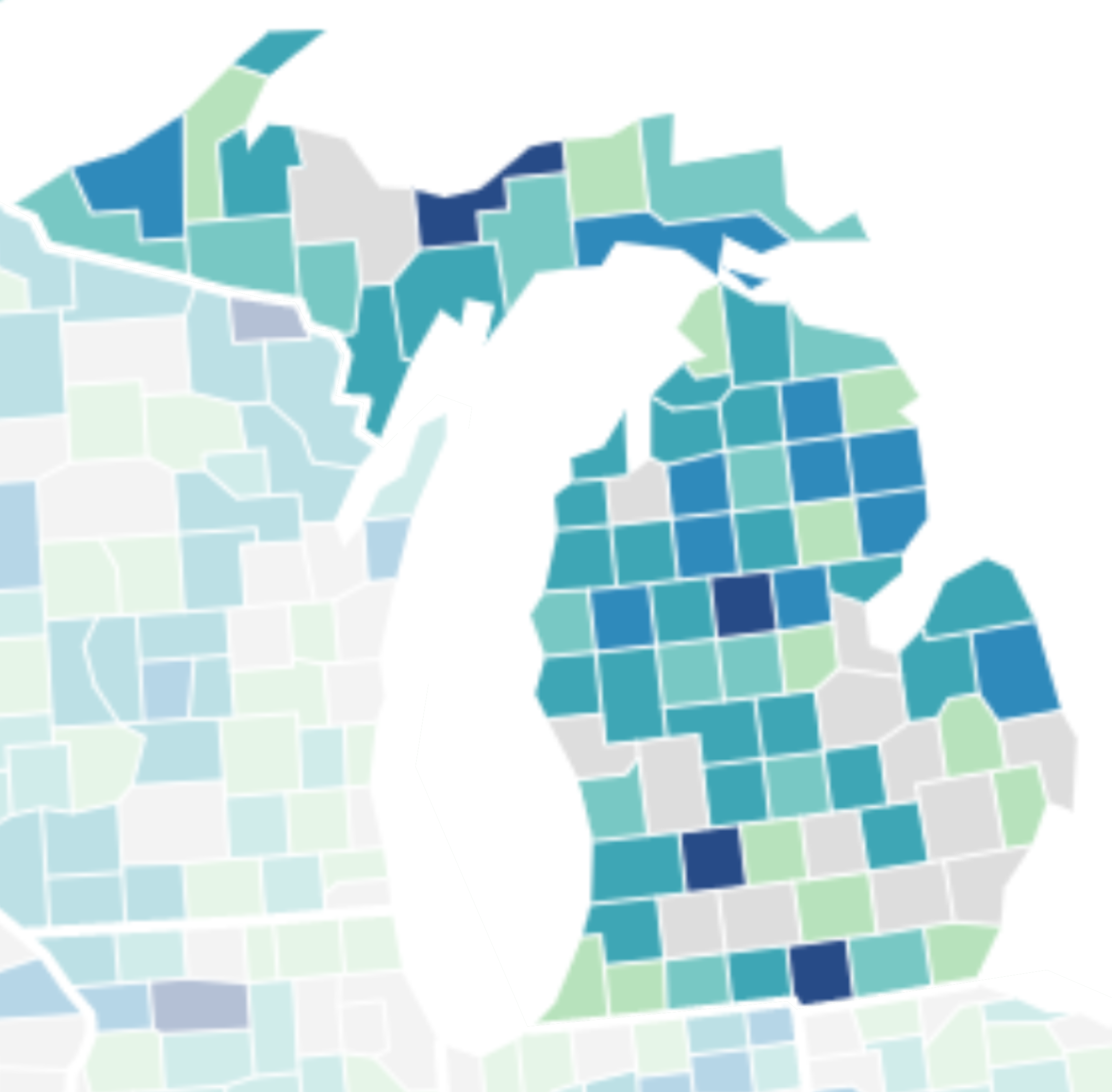
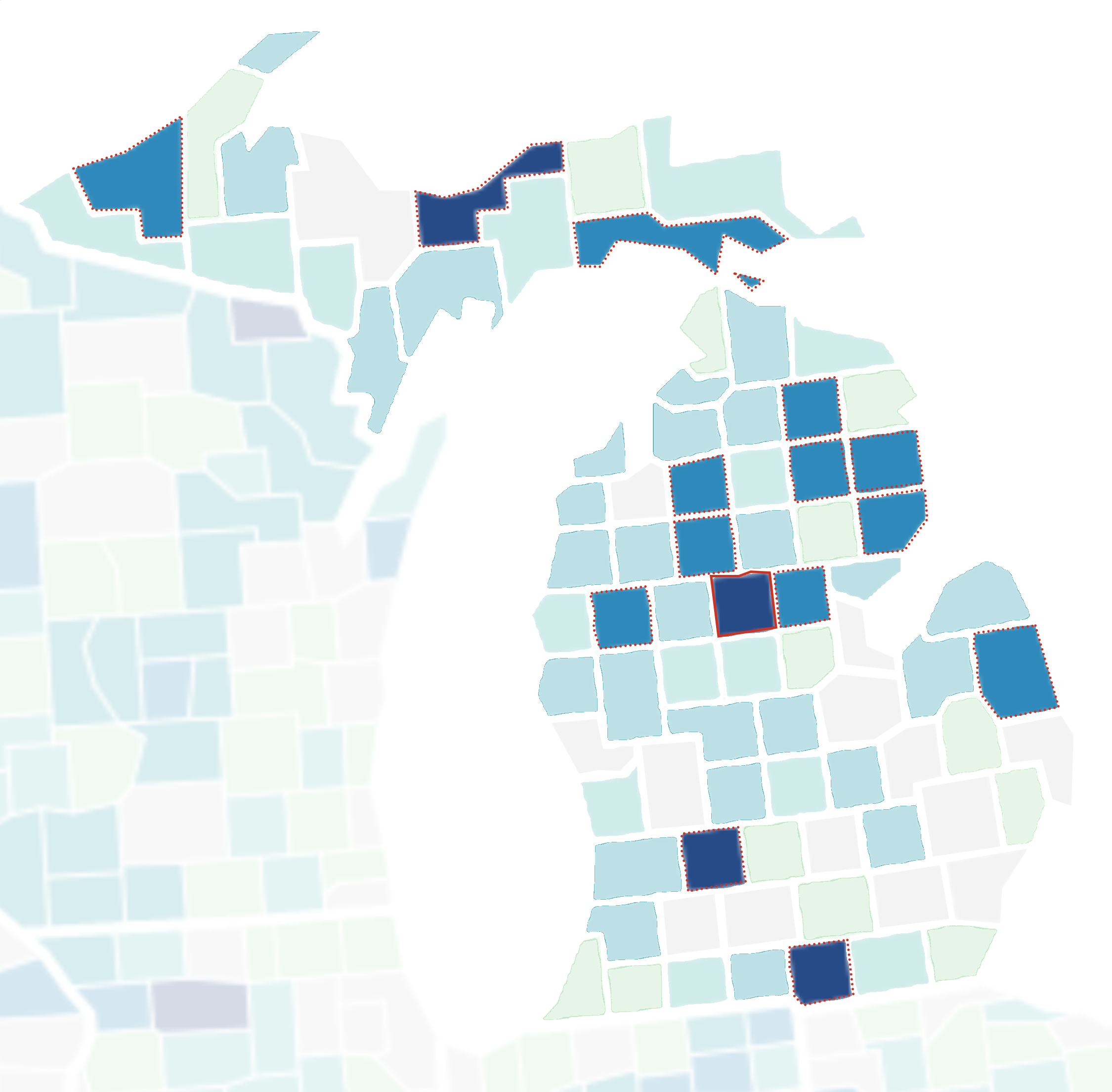
Mapping Healthcare Deserts in Michigan
What
To address the healthcare desert scenarios we identified in our research, we developed a series of physical interventions. Our three physical elements are augmented by our digital intervention: an app that we’ve developed. Each physical intervention is equipped with a wifi hotspot which can work in tandem with the app and encourage more interaction with Health Connect. Now we will walk through each intervention in more detail.
Our smallest-scale physical intervention makes use of space where people already wait in their daily lives and turns waiting time into a healthcare opportunity. Kiosks will be installed in natural waiting areas like grocery stores, laundromats, or bus stops. These kiosks will allow people to schedule appointments, update their health information, or chat with providers. This is most appropriate for low level deserts to create connections between existing healthcare infrastructures.
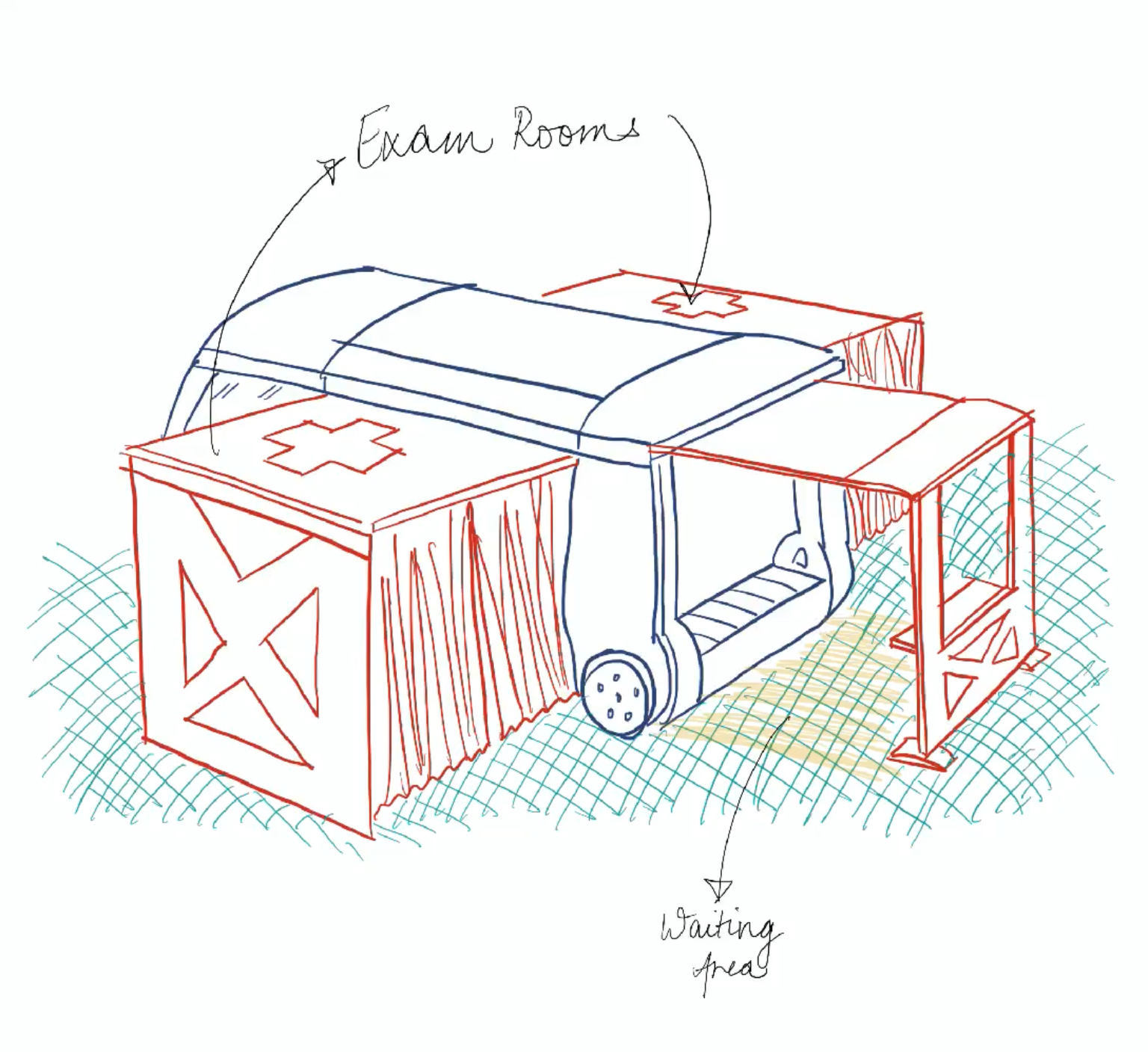
As we scale up in physicality and healthcare need, we move to our mobile intervention. These clinics take primary care to areas of highest need and provide care across various health disciplines: from vaccination stations, to pediatric pop-ups. Services would not necessarily be limited to medical needs, as these interventions could host classes on insurance and technology literacy. This would be most appropriate for medium level deserts to fill in gaps in communities with less substantial healthcare infrastructure.
Our final intervention is for communities with the highest level of healthcare need. For these communities, established infrastructure is either poor or nonexistent, and our intervention would involve construction of new clinics. This newly built infrastructure would be sited in a location with high local utilization to eliminate access issues. For example, a clinic could be sited near a school to provide care for sick children and make access easier for parents if they also need to see a doctor.
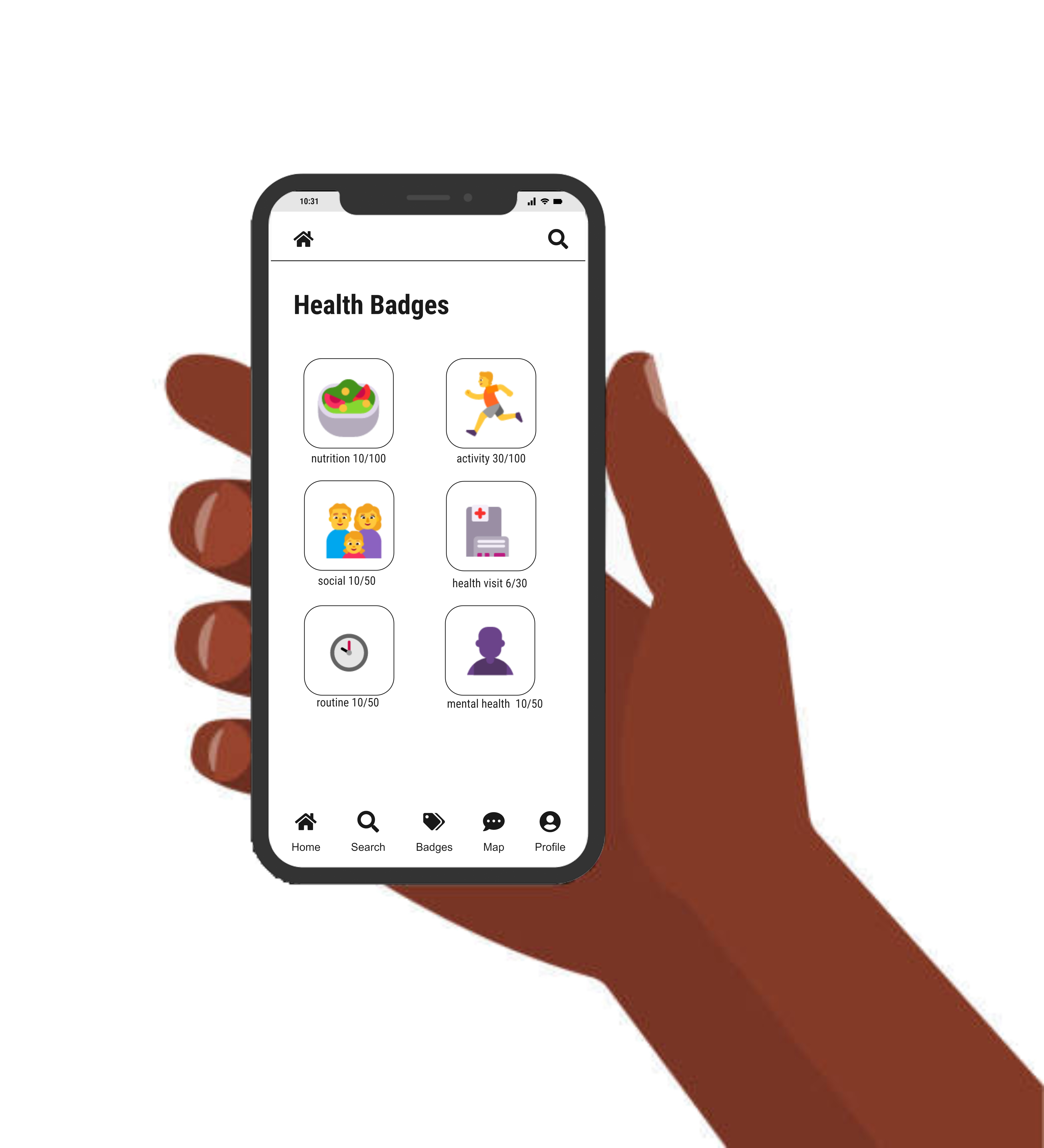
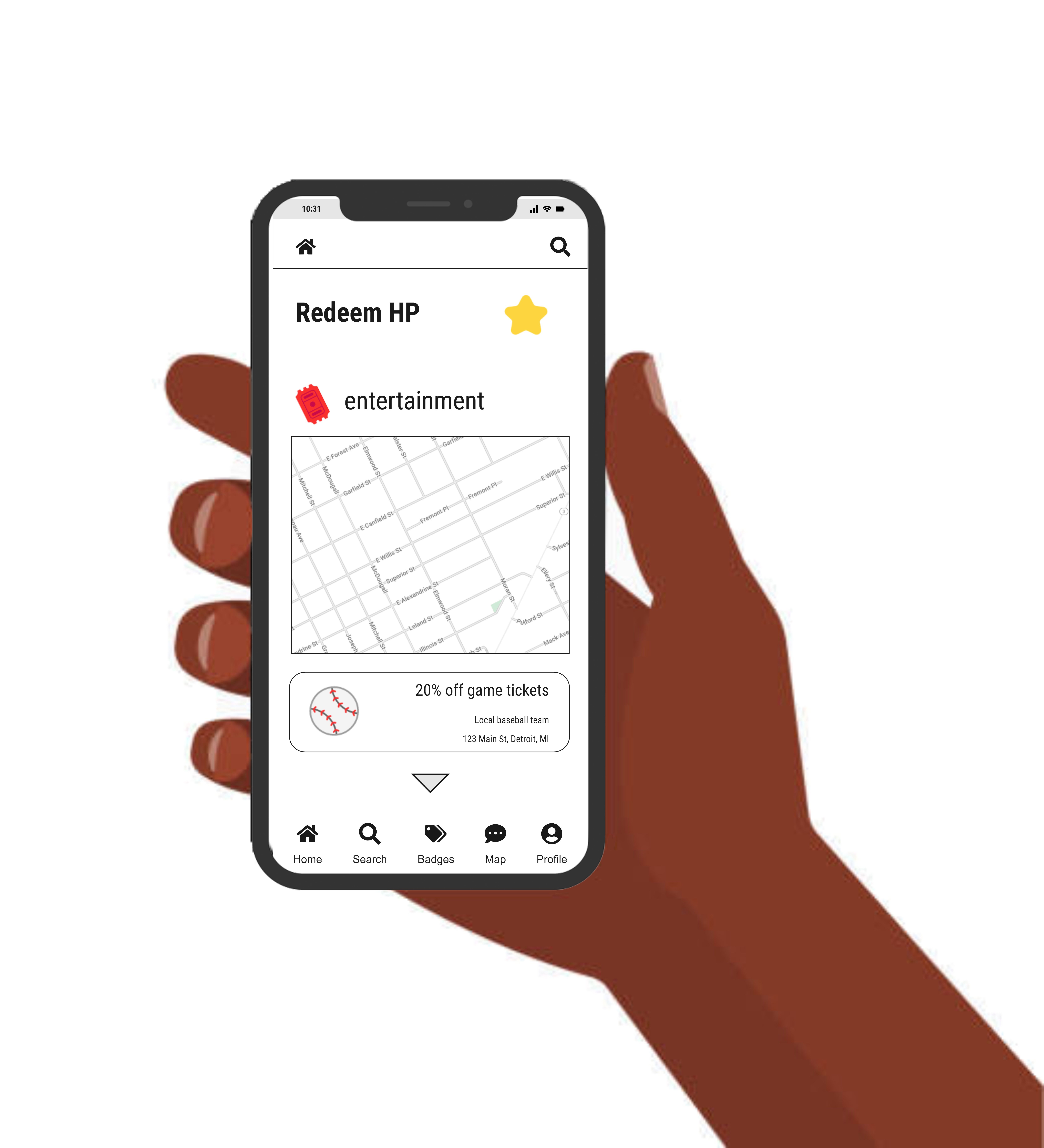
The digital element of our healthcare ecosystem is WebWell by Health Connect. This mobile app supports our physical interventions and promotes healthy and connected lifestyles for its users. Elements of the app address its three guiding principles: health behaviors, social connection, and environmental health. For example: badges, points, and check-ins foster better health behaviors while local events and digital buddies encourage social connectivity beyond the digital sphere.To further the environmental health of a community, geolocations are leveraged to notify users of Health Connect’s physical intervention locations.
The digital interface will provide a platform for information sharing and engagement among community members. People will be able to connect with individuals they already know and be encouraged to interact with new community members in the physical realm. Through information about local events, This point system will provide rewards for individuals, providing positive affirmations that encourage habitual healthy behavior. This intervention will also monitor health behaviors, providing feedback and insight into each user's personal health goals. This project aims to develop a digital platform that creates connections and encourages healthy habits to improve health outcomes and reduce disparities in these underserved communities.
Physical Interventions




Digital Interface
So What
By creating an expanded network of opportunities for connection and health services, underutilized areas in underserved communities will be transformed to create better social connections and health outcomes. This network will encourage community members to engage with their neighborhood and neighbors by providing easily accessible information and hyper-localized program options. These interventions will promote a wide range of healthy lifestyle behaviors. The proposal will encourage digital and physical interaction, each creating a feedback loop, furthering and encouraging engagement.
Physical interventions will activate underutilized urban, suburban, and rural spaces in the pursuit of health-centric communities. The digital connections within the community will encourage potentially isolated populations to attend healthcare-related spaces and events.

Building Block of Health Connect Interventions
Design To Outcomes
Ultimately, we aim for our physical and digital interventions to work together to promote healthy, connected communities. Health Connect will provide increased access to resources, with a firm grounding in addressing the Social Determinants of Health. We seek to leverage these Social Determinants to empower each individual in the community to take an active role in making healthier choices. By establishing a hub of services designed to meet the current and future needs of the community, this initiative will create positive, lasting change in the health outcomes of underserved populations.
Links to Follow:
︎︎︎Two Page Report
︎︎︎Miro Board
︎
Works Cited
- “Assets.ctfassets.net.” Accessed December 8, 2022. https://assets.ctfassets.net/4f3rgqwzdznj/1XSl43l40KXMQiJUtl0iIq/ad0070ad4534f9b5776bc2c41091c321/GoodRx_Healthcare_Deserts_White_Paper.pdf.
- “Assets.ctfassets.net.” Accessed December 8, 2022. https://assets.ctfassets.net/4f3rgqwzdznj/1XSl43l40KXMQiJUtl0iIq/ad0070ad4534f9b5776bc2c41091c321/GoodRx_Healthcare_Deserts_White_Paper.pdf.
- “Brighton Real Estate - Homes for Sale.” Brighton Real Estate - Homes for Sale. Accessed December 8, 2022. https://www.realestateone.com/community/mi/livingston-county/brighton/.
- “Change Systems.” Care Share Health Alliance, November 3, 2020. https://www.caresharehealth.org/partner-for-systems-change/.
- “City Health Dashboard.” City Health Dashboard, October 15, 4687. https://www.cityhealthdashboard.com/.
- “Civic Commons.” Studio Gang. Accessed December 8, 2022. https://studiogang.com/project/civic-commons.
- “Community Health Workers.” County Health Rankings & Roadmaps. Accessed December 8, 2022. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/community-health-workers.
- Constine, Josh. “Kitestring, the App That Makes Sure You Get Home Safe.” TechCrunch, April 16, 2014. https://techcrunch.com/2014/04/16/kitestring/.
- “Container to Clinic: Um-Designed Pop-up Clinic a First-of-Its Kind in Jamaica: GlobalReach: Michigan Medicine.” GlobalReach, January 27, 2020. https://medicine.umich.edu/dept/globalreach/news/archive/201611/container-clinic-um-designed-pop-clinic-first-its-kind-jamaica.
- “Containers 2 Clinics.” Stack + Co. Accessed December 8, 2022. https://stackac.com/projects/containers-2-clinics/.
- “Free Vectors, Stock Photos & PSD Downloads.” Freepik. Accessed December 8, 2022. https://www.freepik.com/.
- “Health Care Services for Uninsured Final Report - Nciom.org.” Accessed December 8, 2022. https://nciom.org/wp-content/uploads/2017/07/HealthCareServicesforUninsured_FinalReport.pdf.
- “Home.” Kindbody, October 25, 2022. https://kindbody.com/.
- “Homeless Pets Get Care at Pop Up Clinic: KCRW Features.” KCRW. KCRW, June 29, 2018. https://www.kcrw.com/news/shows/kcrw-features/homeless-pets-get-care-at-pop-up-clinic.
- “How Do Mobile Health Clinics Improve Access to Health Care?” School of Public Health, September 15, 2022. https://publichealth.tulane.edu/blog/mobile-health-clinics/.
- Lily Bohlke, Michigan News Connection. “Report: Mobile Health Clinics Reach Vulnerable Michigan Communities.” Detroit Metro Times. Detroit Metro Times, June 5, 2022. https://www.metrotimes.com/news/report-mobile-health-clinics-reach-vulnerable-michigan-communities-29790196.
- “Live Healthy Douglas.” Live Healthy Douglas, February 23, 2018. http://www.healthydouglas.org/.
- Marta. Accessed December 8, 2022. https://www.itsmarta.com/station-soccer.aspx.
- Media, F8. “Medical Clinics Go Mobile with Shipping Containers.” Premier Box, August 10, 2022. https://premiershippingcontainers.com.au/2017/11/01/medical-clinics-go-mobile/.
- "Miss Neighbor Lady" Kathy Mouacheupao hosts "Gatherings" in her St. Paul neighborhood – Creative Exchange, and Can Artist Pop-ups Redefine Health? | Amrank Real Estate. “Connecting Creative Practice to Healthcare through Ready Go Tools at the People's Center Health Services.” Creative Exchange, December 13, 2019. https://springboardexchange.org/ready-go-at-peoples-center/.
- “Mobile Clinics.” Sparrow. Accessed December 8, 2022. https://www.sparrow.org/sparrow-community-health/mobile-clinics.
- “Mobile Fact Sheet.” Pew Research Center: Internet, Science & Tech. Pew Research Center, November 16, 2022. https://www.pewresearch.org/internet/fact-sheet/mobile/.
- “Mobile Fact Sheet.” Pew Research Center: Internet, Science & Tech. Pew Research Center, November 16, 2022. https://www.pewresearch.org/internet/fact-sheet/mobile/.
- Module 3: Program Clearinghouse - RHIhub Community Health Workers Toolkit. Accessed December 8, 2022. https://www.ruralhealthinfo.org/toolkits/community-health-workers/3/program-clearinghouse.
- Nanda, Upali, Dr. Upali Nanda is Global Practice Director, Babak Soleimani, and Babak Soleimani is a Senior Design Researcher at HKS. He uses data from sensors. “Community-Bloc: A Framework for Healthy and Pandemic-Resilient Communities.” HKS Architects, October 26, 2022. https://www.hksinc.com/how-we-think/reports/community-bloc-a-framework-for-healthy-and-pandemic-resilient-communities/.
- “Part of the Downtown Business District.” CardCow.com. Accessed December 8, 2022. https://www.cardcow.com/528617/part-downtown-business-district-harrison-michigan/.
- “Provider Relations - Michigan.” Accessed December 8, 2022. https://www.michigan.gov/-/media/Project/Websites/mdhhs/Folder3/Folder27/Folder2/Folder127/Folder1/Folder227/2009-2016_BBA_Archive.pdf?rev=2d7a2d2efd0f4e2ab534eece62960087.
- “Read the Latest Report.” Driving change in health care delivery | Mobile Health Map. Accessed December 8, 2022. https://www.mobilehealthmap.org/.
- “Reef and Rezilient Put Doctors' Offices in Parking Lots - Fast Company.” Accessed December 8, 2022. https://www.fastcompany.com/90688523/rezilient-reef-mobile-doctors-offices.
- “Serving Latino Communities for over 35 Years.” MHP Salud, November 19, 2022. https://mhpsalud.org/.
- “Social Determinants of Health.” Social Determinants of Health - Healthy People 2030. Accessed December 8, 2022. https://health.gov/healthypeople/priority-areas/social-determinants-health.
- “Technology for Healthcare Collaboration and Communication.” Pager. Accessed December 8, 2022. https://pager.com/.
- United Hospital Fund. “Home.” United Hospital Fund. Accessed December 8, 2022. https://uhfnyc.org/.
- View of there's an app for that: A guide for healthcare practitioners and researchers on smartphone technology. Accessed December 8, 2022. https://ojs3-prod.lib.uic.edu/ojs/index.php/ojphi/article/view/5522/4717.
- Wagner, Jodie. “New Mobile Health Clinic to Deliver Care to County's Homeless.” The Palm Beach Post. Palm Beach Post, September 4, 2018. https://www.palmbeachpost.com/story/news/local/2018/09/03/new-mobile-health-clinic-to/7346309007/.
- Wallace-Wells, Benjamin. “Inequality Intensifies the Coronavirus Crisis in Detroit.” The New Yorker, April 7, 2020. https://www.newyorker.com/news/news-desk/the-coronavirus-and-inequality-meet-in-detroit.